Why did the school nurse file a report when I needed my insulin pump during class? The school nurse pulled the insulin pump out of my backpack and her hands froze when she saw the setting screen.

I didn’t think a nurse’s office could change your whole life.
To me, it was always just a place you went when you had a headache or you scraped your knee in gym class. A place that smelled like alcohol wipes and stale mint gum, where the cots had that crinkly paper that stuck to your skin.
But that day—God, that day—I walked in because I needed my insulin pump, and I walked out knowing the person I lived with had been slowly killing me.
It started in class. I remember the room feeling too bright, like the fluorescent lights had turned into a spotlight that followed me. My mouth was so dry I kept swallowing and nothing happened—like my throat had forgotten how to make saliva. My hands were heavy. My thoughts were slow. Sticky. Like my brain was moving through syrup.
I checked my blood sugar and stared at the number until it blurred.
And climbing.
I raised my hand, told the teacher I needed the nurse, and made the walk down the hallway like I was crossing a football field underwater. Every step felt delayed, like my body was receiving commands a few seconds late.
Nurse Kimberly Strand was at her desk when I came in. She’d been the school nurse at Riverside High for as long as anyone could remember—fourteen years, I found out later. She’d seen everything: asthma attacks, panic attacks, kids fainting in the heat, kids faking sick to skip tests.
But when she looked at me, her face changed immediately.
Not annoyed. Not suspicious.
Concerned.
“Sit,” she said, already standing, already moving. “Right now.”
I sat in the chair across from her desk. My backpack thumped against the floor. I fumbled with the zipper like my fingers belonged to someone else.
“My pump,” I managed. “I—I need to bolus. I can’t think.”
She nodded, calm in that way adults get when they’ve done emergencies before. She reached into my backpack and pulled out my insulin pump.
And then her hands froze.
It was subtle—if you weren’t watching her closely you’d miss it. But I was watching. When you feel like you’re dying, you watch everything. You scan faces the way people scan weather alerts.
Her expression moved through stages in the space of a breath.
Concerned… confused… and then something harder. Something sharper.
Like she’d just seen a warning sign no one else could see.
She turned the pump so the screen faced her. Her thumb hovered, not pressing anything yet.
“When did you last change your basal rate?” she asked.
I blinked. Basal rate. That was the background insulin—what the pump delivered all day and night to keep your blood sugar stable when you weren’t eating. It was one of those settings you didn’t mess with casually. You adjusted it carefully, with your endocrinologist, with data.
“My stepmom did it,” I said. “This morning. Like she always does.”
That’s when Nurse Strand looked at me like she was seeing me for the first time.
Not as a student.
As a patient.
As a kid in danger.
“We need to call your endocrinologist,” she said.
My brain tried to catch up. “Why?”
She didn’t answer immediately. She turned to her phone and started dialing, her movements fast but controlled. She kept her voice low—professional, careful—but I was right there, and I heard enough to feel ice slide down my spine.
She used words like dangerous settings.
Then: This doesn’t make medical sense.
Then, the phrase I didn’t understand at the time, but would later wish I’d never learned:
“Possible Munchausen by proxy.”
I remember staring at the posters on her wall—one about washing your hands, another about flu symptoms—while my body buzzed with that awful combination of exhaustion and panic.
She stepped out of the room for a moment, closing the door behind her.
I sat alone, my pump still on her desk, my blood sugar still climbing, and this sick thought kept repeating in my mind:
What did she see? What did she see that I didn’t?
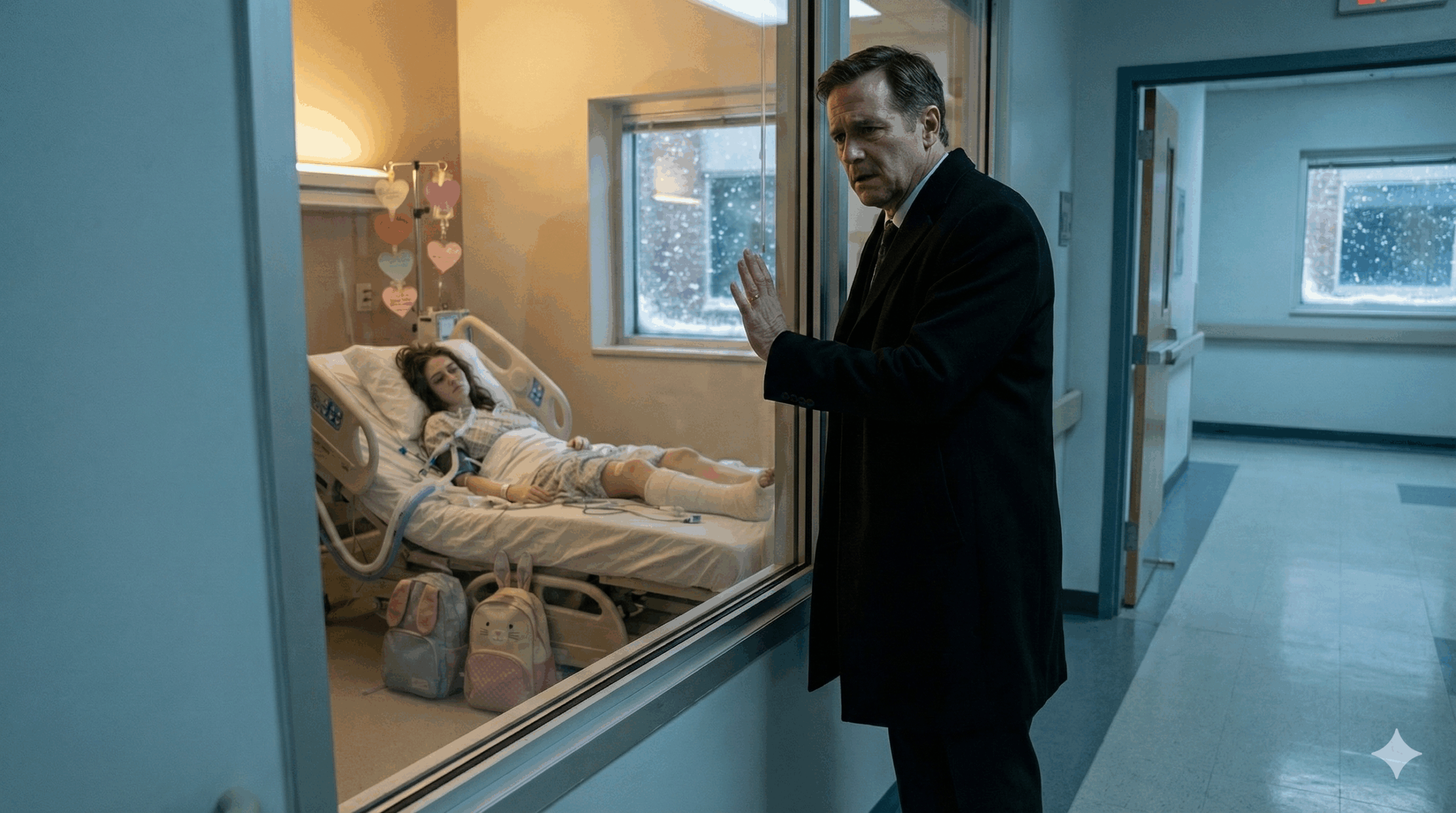
Twenty minutes later, there was a knock at the door.
Not a student knock. Not a teacher knock.
A knock that sounded official.
Nurse Strand opened it, and a woman I’d never seen before stepped in. She wore a plain blazer, carried a folder, and had the kind of expression that didn’t soften even when she tried.
“Hi,” she said gently. “I’m with child protective services.”
My heart did something weird—like it dropped, then floated, then dropped again.
CPS was something you heard about in health class. Something that happened to other families. To kids who showed up with bruises or didn’t have food.
Not… me.
Not a diabetic kid who just needed insulin.
The investigator looked at Nurse Strand, then at me.
“I’m sorry,” she said, and her voice was kind, which somehow made it worse. “But you won’t be going home this afternoon.”
I tried to stand. My legs didn’t cooperate. I gripped the chair.
“What?” I croaked. “Why? I didn’t do anything.”
“You didn’t,” she said quickly. “This isn’t about what you did.”
She took a breath, like she was choosing each word carefully.
“It’s about what’s been done to you.”
I heard Nurse Strand behind me, her voice steady but tight.
“We have reason to believe your insulin pump settings have been altered in a way that’s been harming you.”
The room tilted. My vision narrowed.
Harming me?
By that point, I’d been living with type 1 diabetes for six years. I’d been diagnosed at eleven—back when I still thought the worst thing that could happen to you was failing a math test or getting picked last in gym.
I remember those two weeks before diagnosis like they’re burned into me.
I was thirsty all the time. Not normal thirsty—desperate, bottomless thirsty. I drank water until my stomach hurt and still felt like my mouth was full of sand. I peed constantly. I ate everything in sight and kept losing weight. I’d wake up exhausted and go to bed exhausted, like my body was running on empty no matter what I did.
My mom—my real mom—noticed. Of course she noticed. She noticed everything.
She took me to our pediatrician, Dr. Waverly, who did one blood test and immediately turned serious.
My glucose was 620.
We didn’t even go home. He sent us straight to the emergency room.
That was the day I learned my pancreas had basically quit. My immune system had attacked my insulin-producing cells, and now I needed synthetic insulin to survive. Forever.
It sounds dramatic when you say it like that, but as a kid, what it felt like was… terrifying, and then routine.
Because my mom made it routine.
She learned everything. She took classes. She joined online groups. She tracked my numbers like a scientist. She set alarms for 2 a.m. checks to catch dangerous lows. She taught me how to count carbs, calculate ratios, recognize symptoms before they got bad.
For three years, it was like we were a team. Me and her against this thing.
By fourteen, I was doing most of it myself. Testing. Logging. Adjusting. My mom supervised, but she trusted me.
And then she died.
Car accident. Rainy night. A semi crossed the median. The police used the phrase “instant,” like that was supposed to be comforting.
It wasn’t.
My whole world split in half. There was life with my mom in it, and life without her, and the second one felt like someone had taken the oxygen out of the air.
My dad was… wrecked. He tried, I think. But grief didn’t just break his heart. It broke his ability to function. We lived in the same house like two ghosts moving around each other.
And because my mom had trained me so well, I kept managing my diabetes on autopilot. Mechanical. Wake up, test, insulin, eat, test, insulin, sleep.
Then, six months after my mom died, my dad started dating.
I wasn’t ready. I hated it. But I also understood something I didn’t want to admit: he was lonely and terrified and trying to survive.
He met Valerie Hawthorne at a grief support group.
She was a widow, she said. Her husband had died of cancer. She spoke softly, made sympathetic faces, acted patient with my quiet, angry teenage grief.
She also mentioned—constantly—that she was a pharmaceutical sales representative.
Like it gave her medical authority.
My dad married her eight months after my mom’s death.
And Valerie moved into our house with an efficient smile and a plan.
At first, her involvement in my diabetes seemed… helpful.
She’d remind me to check my blood sugar. Offer to help count carbs. Ask questions that sounded caring.
And my dad—overwhelmed, confused, scared of making a mistake—was grateful. He didn’t understand ratios or basal insulin or correction boluses. My mom had always handled the hard parts.
Valerie stepping in felt like relief to him.
To me, it felt like someone touching something sacred.
But I told myself to be reasonable. I told myself she meant well. I told myself I’d be off to college in a few years anyway.
The first big change she pushed was switching me to an insulin pump.
I’d been doing injections since diagnosis, and it worked. It wasn’t glamorous, but it kept me alive.
Valerie convinced my dad a pump would be better. More convenient. More precise. She scheduled the appointment with my endocrinologist, Dr. Rachel Inamoto—the same doctor who’d been with me since I was eleven.
Dr. Inamoto agreed a pump could work well for me and explained the training. Both the patient and a caregiver had to complete it.
I did my part easily. I understood insulin.
Valerie took pages of notes in caregiver training, nodding like she was collecting proof of expertise.
At first, the pump really was great. Tiny insulin delivery throughout the day. Boluses for meals. A little device that made my life feel less like a medical routine.
But Valerie wouldn’t let it be mine.
She insisted on reviewing my settings. Every evening. Like a manager checking a subordinate’s work.
If I adjusted anything, she questioned why. If my numbers ran high, she treated it like a personal failure.
Her tone was “concerned,” never openly accusing—but it still made me feel incompetent. Watched. Controlled.
And then… I started feeling worse.
My blood sugar ran high constantly. Not occasional spikes—consistent highs. 250. 300. 350. Every day.
I checked my settings. They looked normal.
But my body didn’t feel normal.
I was thirsty again. Exhausted. Foggy. Like my brain was wrapped in cotton.
I told Valerie something seemed wrong.
And she took over.
“I’ll optimize the settings,” she said, with that confident smile. “You’re clearly struggling.”
She spent an evening “researching,” adjusting my basal rates, explaining she was using her pharmaceutical knowledge to help.
I let her.
Because I was tired. And because grief makes you hungry for any adult who sounds sure of themselves.
But after she adjusted the pump, I got worse.
Not just a little worse. Dangerously worse.
My blood sugar would be in the 400s in the morning even though the pump was supposed to deliver insulin all night. Valerie would frown, act concerned, adjust again.
She started controlling my meals too. Counting carbs for me. Programming boluses herself. Not trusting me to do it.
I hated it, but I was too tired to fight.
And by the time school started in August, I wasn’t just sick.
I was fading.
By junior year, I didn’t feel like a person anymore.
I felt like a body being dragged through days.
I’d sit in class and watch my teachers’ mouths move, but the words didn’t connect to meaning. It was like trying to read through fogged glass. My head ached constantly—this dull, pressurized ache behind my eyes—and my skin felt tight and dry no matter how much water I drank. I was always drinking. Always.
And still, my mouth tasted like cotton.
The bathroom trips were humiliating. I’d raise my hand, whisper “medical,” and shuffle out while people stared. Teachers tried to hide their irritation, but I could feel it anyway. After the third time in one class, even the kind ones started looking like they didn’t believe me.
My friends stopped inviting me to hang out after school because I always said no. Not because I didn’t want to go—but because I couldn’t imagine making it through a normal evening without needing to lie down.
Soccer was the worst. Soccer used to be the one place I felt strong. Like my body belonged to me. Like diabetes was something I managed, not something that managed me.
But suddenly, I couldn’t keep up.
My legs would go heavy halfway through warm-ups, my vision would blur at the edges, and my chest would feel tight, like my lungs were too small for the air. My coach benched me at first “until you’re stable,” he said, the word stable sounding like a distant dream.
Then he cut me.
Not because he was cruel. Because I was a liability. Because if I collapsed on the field with blood sugar in the 400s, it would be an emergency, and everyone knew it.
I told myself it was temporary.
Valerie told me it was my fault.
“You’re not following the plan,” she’d say, tapping her phone where she tracked my numbers like it was a performance report. “Teenage boys are hard to manage. You think you’re invincible, but you’re not.”
I would try to argue. Weakly. “I am following it.”
She’d smile in that calm, superior way. “Then why are your numbers like this?”
And she always had an explanation ready before I could even think.
Stress. Hormones. Growth spurts. “Sneaking soda.” “Not bolusing properly.” “Being careless.”
And the worst part was that I started believing her—because when you feel sick all the time, you get desperate for a reason. Any reason. Even one that makes you hate yourself.
My dad noticed I looked bad. He really did. He’d stare at me across the dinner table like he was trying to solve a puzzle.
But Valerie would slide in smoothly, hand on his arm, voice warm.
“He’s growing,” she’d say. “It’s complicated. I’m handling it.”
And my dad would exhale like he was letting someone else hold a weight he couldn’t carry.
That was the problem.
Valerie didn’t just take over my pump.
She took over the story.
In her story, she was the devoted caregiver. The exhausted stepmother doing her best.
And I was the difficult diabetic kid who didn’t comply.
So when I walked into the nurse’s office for the first time that fall, I didn’t even think it was a big deal.
I just thought: I can’t get my numbers down. I need help.
It was mid-September. Third-period chemistry. The room spun when I stood up, and the nausea hit so hard my mouth filled with saliva like my body was preparing to throw up.
I checked my blood sugar at my desk.
I stared at it, trying to do the math for a correction bolus, but the numbers didn’t hold steady in my mind. Ratios I’d known for years suddenly felt like a foreign language.
So I went to the nurse.
Nurse Strand took one look at me and didn’t ask questions first. She grabbed her meter, tested me herself.
Her eyebrows drew together.
“Let me see your pump,” she said.
I handed it over, and she started scrolling.
I was so sick I didn’t even have the energy to be embarrassed.
Then she asked, “Who programs these settings?”
“My stepmom,” I said, voice thick. “Valerie.”
“And your endocrinologist approved this?” she asked.
I hesitated. Because suddenly I realized… I didn’t know. Valerie always talked to Dr. Inamoto. Valerie always answered questions. Valerie always took control.
“I… I think so,” I said, and even as I said it, I knew it sounded wrong.
Nurse Strand didn’t accuse. She didn’t panic. She just went quiet in a way that made my stomach clench.
She called Valerie.
Valerie arrived within twenty minutes, like she’d been waiting for the chance to prove something. Concerned expression in place. Perfect hair. Soft voice.
“Oh sweetheart,” she said, touching my shoulder like she was the hero arriving to rescue me from my own incompetence. Then she turned to Nurse Strand. “He’s been having terrible control. It’s been so hard. I’ve been trying to optimize his settings.”
Nurse Strand suggested we consult my endocrinologist about the settings.
Valerie agreed instantly—so smoothly it almost looked cooperative.
“Yes, absolutely,” she said. “I was planning to schedule an appointment anyway.”
She took me home.
And in the car, the sweetness dropped. Not fully. Just enough for me to feel the edge.
“You need to stop fighting me,” she said, eyes on the road. “This gets worse when you’re stubborn. Are you drinking soda at school?”
“No.”
“Are you sure?” Her voice went light. “Because your numbers don’t lie.”
That night, she changed my pump settings again.
And after that, I got even worse.
The second visit to the nurse happened in early October.
I was in English when my vision started tunneling. I could hear the teacher’s voice, but it sounded far away, like she was speaking through water. When I tried to stand, the room tilted violently and my knees buckled.
A classmate—thank God for her—walked me down to the nurse.
I collapsed into the chair in Nurse Strand’s office, shaking so hard my teeth clicked.
She tested my blood sugar.
This time, she didn’t just look confused.
She looked angry.
Not at me—at the situation.
She checked my pump settings again. And while I sat there half-conscious, she took out her phone and quietly photographed the screens.
That detail didn’t register until later. At the time, I was just a sick kid trying not to vomit.
She asked me questions. Specific questions.
“How often does Valerie change your settings?”
“Almost every day.”
“Do you know what your old rates were?”
“No.”
“Does she let you manage it yourself?”
“Not really.”
“Do you see your doctors alone?”
I blinked. “No… she’s always there.”
Nurse Strand’s face went still.
Then she said, very gently, “I want to try something.”
She explained she wasn’t going to “take over” my care. She just wanted to test whether the settings made sense. She walked me through a basic calculation based on my weight and activity level—something my mom had taught me years ago.
The number she got was lower than what my pump was currently delivering.
That didn’t make sense to me at first, because I was stuck on the fact that I was high. High meant I needed more insulin, right?
But Nurse Strand explained it in a way my foggy brain could understand: if the pump is set wrong, you can be high for reasons that don’t match the dose—bad ratios, wrong patterns, improper corrections, sabotaged settings. Sometimes “more” doesn’t fix “wrong.” It just makes the body unstable and sick.
She asked if she could adjust my basal temporarily—just for the afternoon while I stayed in her office.
I agreed because I would’ve agreed to anything that made the spinning stop.
She lowered the basal. Not dramatically. Carefully. Then she had me stay, checking my blood sugar every thirty minutes.
For the first time in weeks, the number moved the right direction.
By the end of the day, I was at 256.
Still too high, but… better. Clearer. Like my brain had finally come up for air.
She printed out what she’d done and told me to show my endocrinologist.
Then she asked again, softer this time: “Does Valerie ever stop you from getting help?”
I didn’t know how to answer, because she didn’t “stop” me in an obvious way. She didn’t lock me in a room. She didn’t say “you can’t.”
She just controlled the schedule. Controlled the narrative. Controlled what people believed about me.
That night, Valerie checked my pump settings like she always did.
And when she saw they’d been changed?
Her mask slipped.
Just for a second.
Her eyes went sharp.
“Who touched this?” she demanded.
I told her. “Nurse Strand. She said—”
Valerie cut me off. “She is NOT qualified to do that.”
“She said my numbers—”
“She overstepped,” Valerie snapped, and then forced her voice back into something calm. “Your nurse is not your endocrinologist. She doesn’t understand complex management.”
She changed the settings back immediately. Like she couldn’t stand the idea of someone else touching what she controlled.
Then she went to my dad.
I heard her through the wall, that careful voice, the one she used when she wanted to sound reasonable.
“The school nurse is interfering with his care,” she said. “She’s changing medical settings without consent. That’s dangerous. We need to put a stop to it.”
My dad—my exhausted, grieving dad—believed her.
He emailed the principal.
He asked that Nurse Strand not adjust anything without parental consent.
And in doing that, he unknowingly helped Valerie tighten her grip.
My blood sugar stayed high.
Late October, I’d lost weight. My clothes hung weird. My cheekbones looked too sharp. I’d wake up at night drenched in sweat and stumble to the bathroom, vision blurred, heart racing.
I told my dad, “I need to see Dr. Inamoto. Now.”
Valerie smiled like I was being dramatic. “We have an appointment next month.”
“I can’t wait,” I said, voice cracking. “I feel like I’m dying.”
Valerie’s eyes flicked to my dad. She put on her concerned face like a costume. “He’s anxious,” she said gently. “Teenagers catastrophize.”
My dad looked torn.
And that hurt more than the symptoms.
Because I needed him to believe me.
I needed him to choose me.
Finally, after another night of me shaking and vomiting and crying out of pure exhaustion, my dad scheduled an emergency appointment.
The appointment that should have fixed everything.
The one that instead opened the door to a nightmare.
Dr. Inamoto took one look at me and her professional composure cracked.
“You’ve lost a lot of weight,” she said immediately. “What is going on?”
Valerie answered first, of course. She always did.
“He’s been struggling,” Valerie said. “It’s been so difficult. I’ve been adjusting the pump to optimize—”
Dr. Inamoto held up a hand. “Let’s download the pump data.”
When she plugged in the pump and the screen filled with graphs and settings histories, the room went quiet in a way that made my skin prickle.
Dr. Inamoto scrolled.
Her eyes narrowed.
She asked, very slowly, “Who has been changing these settings?”
Valerie straightened. “I have, with my pharmaceutical background—”
“These changes don’t reflect standard diabetes management,” Dr. Inamoto said, voice controlled. “They reflect… chaos.”
Valerie’s smile twitched. “He’s not compliant. He lies about what he eats.”
Dr. Inamoto turned to me. “Do you program your own boluses?”
I swallowed. “Not anymore. Valerie does.”
Dr. Inamoto’s jaw tightened. “Has anyone checked ketones?”
Silence.
Valerie opened her mouth, then closed it.
Dr. Inamoto pulled out a urine ketone strip and had me test right there.
The strip turned dark purple almost instantly.
Dr. Inamoto looked at my dad. “He is in diabetic ketoacidosis. He needs the ER now.”
Valerie protested—of course she did.
“I can manage him at home,” she said quickly. “This is overreacting—”
Dr. Inamoto’s voice snapped sharp. “No. He could go into a coma.”
And the strangest part?
When Valerie argued, I didn’t just hear defensiveness.
I heard… annoyance.
Like my near-death emergency was inconvenient to her plan.