My Son Called Me Crying From The Er At 3:47 A.M., Saying The Doctor Thought He Was Faking It. I Drove There Half-Dressed And Furious—Until The Ct Results Came In And The Entire Room Went Quiet. His Appendix Had Already Ruptured…

My son called from the hospital.
“Dad, the doctor is refusing to treat me and says I’m faking my symptoms for drugs.”
When I arrived at the ER, the doctor’s smug expression disappeared and he whispered, “Chief of Surgery… I didn’t realize he was your son.”
The call came at 3:47 a.m. on a Friday morning while I was reviewing surgical schedules for the upcoming week. My son Ethan’s name flashed on my phone screen and my chest immediately tightened.
Ethan was 22, a grad student at State University three hours away, and he never called at this hour unless something was seriously wrong.
“Dad, I’m at Mercy General’s ER.”
His voice was strained, tight with pain.
“I’ve been here for two hours, and the doctor won’t treat me. He keeps saying I’m faking my symptoms to get painkillers. Dad, something’s really wrong. It hurts so bad I can barely stand.”
I was already grabbing my keys.
“What symptoms? Tell me exactly what you’re feeling.”
He took a shaky breath.
“Started around midnight. Sharp pain in my lower right abdomen. It’s gotten worse every hour. I’m nauseous. Threw up twice. I have a fever.”
He swallowed hard.
“I tried to explain my symptoms, but the doctor just kept asking about my drug history, looking at me like I’m some junkie.”
My hands went cold.
Lower right quadrant pain, nausea, vomiting, fever. Classic appendicitis presentation.
If it was appendicitis and they weren’t treating him, his appendix could rupture. That meant sepsis, peritonitis, potential death.
“Who’s the attending physician?” I demanded.
“Dr. Vance. Dr. Leonard Vance.”
Ethan’s breathing hitched.
“He won’t even examine me properly. He did this quick palpation, barely touched my abdomen, then told the nurse to give me Tylenol and discharge me. Dad, I’m not making this up. Something’s wrong.”
I was already in my car, backing out of the driveway.
“Don’t let them discharge you. Tell them your father is Dr. Garrison Mills, Chief of Surgery at St. Catherine’s Hospital, and I’m on my way. Do not leave that ER, Ethan.”
My grip tightened on the steering wheel.
“If your appendix ruptures because they delayed treatment, people are going to lose their medical licenses.”
I’d been Chief of Surgery at St. Catherine’s for eight years, a general surgeon for twenty-three years before that. I’d seen every complication, every delayed diagnosis, every case of medical negligence that ended in tragedy.
And one of the things that made my blood boil was when doctors let their biases override their clinical judgment.
Young male patients presenting with abdominal pain were often dismissed as drug seekers, especially if they had tattoos, piercings, or looked like they might use recreational substances.
Ethan had both arms sleeved with tattoos, wore his hair long, and had a nose ring. He looked like the stereotype that lazy doctors use to justify not doing their jobs.
But Ethan was also brilliant, kind, and had never touched hard drugs in his life. He was finishing his master’s in environmental science and spent his weekends volunteering at wildlife rehabilitation centers.
The idea that some arrogant ER doctor had taken one look at my son and decided he was a drug addict without doing proper diagnostic work made me want to put my fist through something.
The drive to Mercy General took me two hours and thirty-eight minutes. I spent the entire time on the phone, first with Ethan to keep him calm and monitor his symptoms, then with colleagues to gather information about Dr. Leonard Vance.
What I learned made my stomach turn.
Vance was 46, had been an ER physician for fifteen years, and had multiple complaints filed against him by patients who claimed he’d dismissed their symptoms and provided inadequate care.
Nothing had stuck because the hospital administration kept settling complaints quietly, and the medical board had never pursued formal investigation.
He had a reputation among nurses as being dismissive, arrogant, and quick to label patients as drug seekers without proper assessment.
One of my colleagues, Dr. I. Simmons, who’d worked with Vance years ago, told me bluntly, “Garrison, Vance is a lazy doctor who’s coasting on his credentials. He profiles patients based on appearance and makes snap judgments without doing the diagnostic work. I’ve heard he’s particularly bad with young men. Assumes they’re all addicts looking for a fix.”
By the time I pulled into Mercy General’s parking lot at 6:31 a.m., Ethan had been in the ER for nearly five hours without treatment.
Five hours with potential appendicitis. Five hours during which his appendix could have ruptured.
I walked through those ER doors with my hospital ID badge visible and my fury carefully controlled.
I found Ethan in a curtained area in the corner, looking pale and sweaty, curled on his side on the gurney. A nurse was checking his vitals and she looked worried.
“Sir, are you family?” she asked when she saw me approach.
“I’m his father,” I said. “Dr. Garrison Mills, Chief of Surgery at St. Catherine’s.”
Her eyes widened slightly.
“I’ve been concerned about him. His fever’s gone up to 102.3 and his pain level keeps increasing. I’ve asked Dr. Vance twice to reassess, but he keeps saying the patient is exhibiting drug-seeking behavior.”
I looked at my son. His skin had a grayish tint and he was holding his right side protectively.
Classic peritoneal signs.
“Ethan, I need you to try to straighten out for me.”
He tried and gasped in pain.
“Can’t. Hurts too much.”
I did a gentle palpation of his abdomen. The moment I touched the right lower quadrant, he nearly came off the table.
Rebound tenderness, guarding, fever, five-hour history of progressive pain.
This wasn’t just appendicitis.
This was likely a ruptured appendix.
“Where’s Dr. Vance?” My voice came out colder than I’d intended.
The nurse hesitated. “He’s with another patient. Room 4.”
I pulled back the curtain and walked straight to Room 4.
Through the open doorway, I could see a man in his mid-40s wearing scrubs and a white coat, laughing with another physician while reviewing a chart. He had the casual arrogance of someone who’d never faced real consequences for his actions.
“Dr. Vance.”
He turned, his expression still amused from whatever he’d been laughing about.
“Yes? Are you a family member of a patient?”
“I’m Dr. Garrison Mills,” I said, “Chief of Surgery at St. Catherine’s Hospital. I’m also the father of Ethan Mills—the young man you’ve been refusing to treat for the past five hours, despite clear symptoms of acute appendicitis.”
I watched his face change.
The amusement vanished first, replaced by confusion, then recognition as my name and title registered.
His face went white.
“Chief of Surgery,” he whispered. “I didn’t realize… He said his name was Ethan Mills. I didn’t connect…”
“You didn’t connect that Mills is a common surname,” I said, “and that even if you had, it wouldn’t matter. You’re a physician. Your job is to assess and treat patients based on their symptoms, not make assumptions based on how they look.”
My voice was quiet, but every word landed like a hammer.
“My son presented with right lower quadrant pain, nausea, vomiting, and fever. That’s appendicitis until proven otherwise. Instead of ordering labs, imaging, and proper assessment, you labeled him a drug seeker and prescribed Tylenol.”
I held his gaze.
“Do you understand what you’ve done?”
Vance tried to recover, pulling himself up to his full height.
“Mr. Mills presented with vague complaints and a history inconsistent with serious pathology. His pain level seemed exaggerated, and he specifically asked for narcotic pain medication, which is a red flag for drug-seeking behavior.”
“Did he ask for narcotics,” I said, “or did he ask for pain relief after sitting in your ER for hours in agony?”
I stepped closer.
“Did you run labs? Did you order a CT scan? Did you perform a proper physical exam with assessment for peritoneal signs?”
I didn’t raise my voice. I didn’t need to.
“Or did you take one look at a young man with tattoos and decide he was a drug addict?”
Vance’s jaw tightened.
“I used my clinical judgment based on fifteen years of experience. Not every patient with abdominal pain needs extensive imaging. We’d go bankrupt ordering CTs for everyone who comes in claiming to have pain.”
“Clinical judgment requires actual clinical assessment,” I said. “Show me his chart.”
Vance hesitated, then pulled up Ethan’s file on the computer.
I scanned it quickly and felt my hands start to shake with rage.
Vital signs documented: elevated temperature, elevated heart rate, elevated respiratory rate. All signs of systemic illness.
Physical exam notes: Patient states he has abdominal pain. Mild tenderness noted on palpation. No obvious acute pathology. Patient appears to be exaggerating symptoms. Likely drug-seeking behavior. Prescribed acetaminophen 500 mg and recommended discharge.
That was it.
No complete abdominal exam documented. No assessment for rebound tenderness, rigidity, or guarding. No labs ordered, no imaging, no differential diagnosis listed.
Just a dismissive assumption and a prescription for over-the-counter Tylenol.
“This isn’t a medical assessment,” I said quietly. “This is malpractice.”
Vance’s face flushed.
“Now, wait just a minute. You can’t come into my ER and start making accusations. I’m an experienced physician and I made a judgment call based on the patient’s presentation.”
“You made a prejudiced assumption based on his appearance,” I said. “There’s a difference.”
I pulled out my phone.
“I’m calling Dr. Whitmore—the Chief of Emergency Medicine here—and I’m requesting an immediate surgical consult for my son. Then I’m filing a formal complaint with the state medical board about your negligent care.”
I walked back to Ethan’s area and found him trying to sit up, his face twisted in pain.
“Dad, it’s getting worse. It really hurts.”
I put my hand on his shoulder.
“I know. We’re getting you help right now.”
I called Dr. Andrea Whitmore, who I knew professionally from medical conferences. She answered on the third ring, her voice sharp with the alertness of someone used to crisis calls.
“Dr. Mills. What’s going on?”
I explained the situation in clinical terms.
“Twenty-two-year-old male. Five-hour history of progressive right lower quadrant pain. Fever. Nausea. Vomiting. No diagnostic workup completed. Symptoms consistent with acute appendicitis, possibly with rupture.”
She was silent for a moment, then said something sharp under her breath.
“I’m twenty minutes away. I’m calling in Dr. Raymond Kowalski from general surgery to assess immediately.”
Her voice tightened.
“And Garrison… I’m sorry. Vance has been a problem for a while, but we haven’t had enough documented incidents to take action. This might be what we need.”
Kowalski arrived within fifteen minutes. He was young, maybe early 30s, with the intense focus of a surgeon who took his job seriously.
He introduced himself to Ethan, explained what he was going to do, and performed a thorough abdominal exam.
His expression grew progressively more concerned.
“Significant rebound tenderness, guarding, rigidity. McBurney’s point is exquisitely tender.”
He looked at Ethan, then at me.
“With the five-hour symptom progression and elevated fever, I’m very concerned about perforation.”
He straightened.
“We need labs stat and an abdominal CT with contrast. But honestly, based on clinical presentation, this is almost certainly appendicitis. The delay in treatment is concerning.”
The CT results came back forty-three minutes later, and they confirmed the nightmare scenario: ruptured appendix with signs of early peritonitis—free fluid in the abdomen, inflammatory changes throughout the right lower quadrant.
Ethan needed emergency surgery immediately.
Dr. Whitmore had arrived by then, a tall woman in her 50s with steel-gray hair and an expression of barely controlled fury.
She reviewed the CT images, then turned to where Vance was standing near the nurse’s station, trying to look busy.
“Dr. Vance. My office. Now.”
Then she looked at me.
“Dr. Mills, we’re taking your son to surgery immediately. Dr. Kowalski will be the attending surgeon, and I’m bringing in Dr. Lisa Chen.”
She caught herself.
“Dr. Lisa Warren—one of our best general surgeons—to assist. Your son is going to be fine, but this should never have happened.”
They wheeled Ethan to surgery at 8:15 a.m., nearly seven hours after his symptoms had started.
I walked alongside the gurney, holding his hand.
“Dad, I’m scared,” he said quietly.
“I know,” I said. “But you’re in good hands. Dr. Kowalski is excellent, and they’re going to fix this. You’re going to be fine.”
He squeezed my hand.
“I wasn’t making it up. I wasn’t faking for drugs.”
My throat tightened.
“I know you weren’t. This is not your fault. None of this is your fault.”
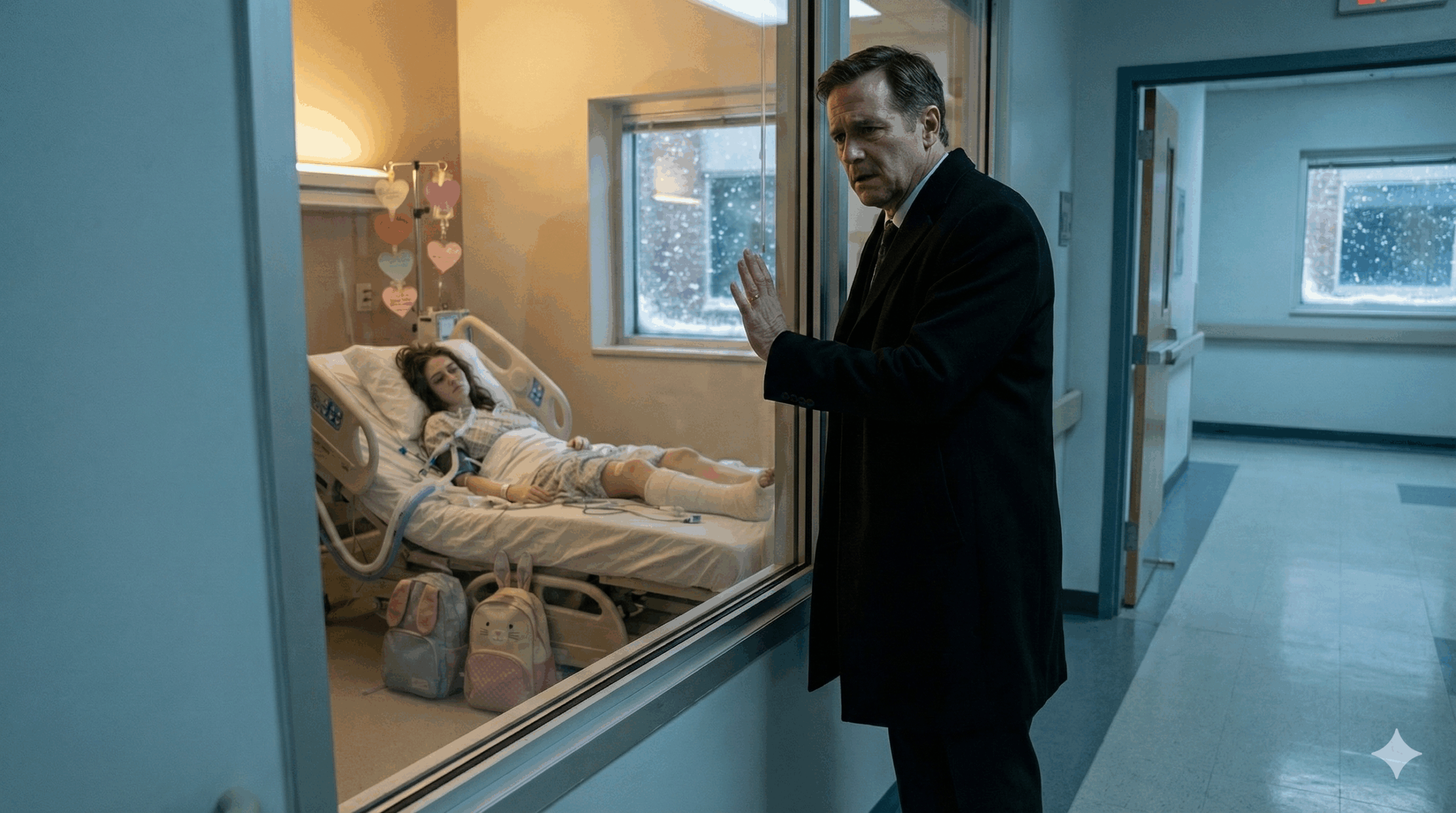
They took him through the surgical suite doors and I was left standing in the hallway, watching through the small windows as they prepped him for surgery.
My hands were shaking.
My son had nearly died because a doctor had let his prejudices override his medical training.
I pulled out my phone and started making calls.
First to my ex-wife—Ethan’s mother—who deserved to know what was happening. She answered immediately, her voice thick with sleep.
“Garrison, what’s wrong?”
I explained everything: the ER visit, Vance’s dismissal, the delayed diagnosis, the emergency surgery.
By the time I finished, she was crying.
“He could have died if you hadn’t gone there. If he’d listened to that doctor and gone home, he could have died.”
“I know,” I said, my voice rough. “But he didn’t. He’s in surgery now, and he’s going to be okay.”
“I’m getting on the next flight,” she said. “I’ll be there in six hours.”
After we hung up, I called my attorney, Jeffrey Hartman, who specialized in medical malpractice cases. I’d known Jeffrey for fifteen years and had served as an expert witness on several of his cases.
He answered with the professional alertness of someone used to emergency calls.
“Garrison, what’s happened?”
I laid out the timeline: the symptoms, the lack of diagnostic workup, the delayed treatment, the ruptured appendix.
Jeffrey listened without interrupting, and I could hear him typing notes.
“This is clear-cut negligence,” he said when I finished. “Failure to diagnose, inadequate assessment, delay in treatment resulting in serious harm.”
His voice sharpened.
“The fact that the patient was profiled based on appearance adds another dimension. We can file a formal complaint with the state medical board. And depending on the outcome of your son’s surgery and recovery, there may be grounds for a civil suit.”
“I want more than a complaint,” I said. “I want Vance’s license reviewed. I want a full investigation into his practice patterns. And I want to make sure this never happens to another patient.”
Jeffrey was quiet for a moment.
“You’re asking for a war, Garrison. The hospital will protect him. The medical board moves slowly. This could take years.”
“I don’t care how long it takes,” I said. “My son nearly died because a doctor was too lazy and prejudiced to do his job. That’s unacceptable.”
“Then we’ll do it,” Jeffrey said. “But we need documentation. Everything. Medical records, witness statements, timeline of events. I’ll start the paperwork today.”
The surgery took three hours and twenty-two minutes.
Dr. Kowalski came out looking exhausted, but satisfied.
“The appendix had ruptured, as we suspected. There was significant contamination in the peritoneal cavity. We performed an appendectomy, irrigated extensively, and placed drains.”
He exhaled.
“He’s going to need IV antibiotics for several days and close monitoring, but he should make a full recovery.”
I felt my knees go weak with relief.
“Thank you.”
Kowalski’s expression hardened.
“Dr. Mills, I need to be honest with you. The rupture was recent—probably within the past two to three hours. If he’d been assessed and treated when he first arrived at the ER, we could have performed the surgery before perforation occurred.”
He didn’t look away.
“The delay directly caused the rupture and the complications.”
“I know,” I said.
“I’m documenting everything in my surgical notes,” he continued. “The timeline, the delayed diagnosis, the preventable perforation. If you pursue this legally or through the medical board, I’ll testify to the standard of care violations.”
I shook his hand.
“I appreciate that more than you know.”
Ethan woke up in recovery around 1:30 p.m., groggy from anesthesia but stable.
I sat next to his bed, watching the monitors, counting his breaths.
He opened his eyes slowly and looked at me.
“Dad?”
“I’m here,” I said. “Surgery went well. They removed your appendix and you’re going to be fine.”
His eyes filled with tears.
“I thought I was going crazy. Vance kept saying I was faking, that I just wanted drugs. I started wondering if maybe I was making it up, if the pain wasn’t real.”
I took his hand.
“The pain was real. You had a ruptured appendix. You were right to trust your body. Vance was wrong, and he’s going to face consequences for what he did.”
Over the next three days, while Ethan recovered in the hospital, I documented everything.
I requested copies of all his medical records from the ER visit and the surgery. I interviewed the nurses who’d been on duty during his ER stay.
What I found made me even angrier.
Three different nurses had expressed concerns to Dr. Vance about Ethan’s condition.
One nurse, a woman named Carol Brennan with twenty-six years of ER experience, had specifically told Vance that Ethan’s vital signs and symptom progression were concerning and suggested labs and imaging.
Vance had dismissed her concerns with a condescending comment about how nurses needed to trust physician judgment.
Another nurse, David Kim, had documented in his nursing notes that the patient appeared to be in significant distress and that his pain seemed genuine, not exaggerated.
Vance had ignored these assessments.
I also discovered that Ethan wasn’t the first patient Vance had dismissed.
In the past eighteen months, there had been four formal complaints filed against him by patients or family members alleging inadequate care.
One case involved a young woman with chest pain who Vance had diagnosed with anxiety and sent home. She’d returned six hours later with a pulmonary embolism.
Another involved a teenage boy with abdominal pain that Vance dismissed as gastritis. It was actually a perforated ulcer.
The hospital had settled both cases quietly with non-disclosure agreements.
No disciplinary action had been taken against Vance.
Dr. Whitmore called me on the fourth day of Ethan’s hospitalization.
“Dr. Mills, I wanted to update you personally. I’ve initiated a formal peer review of Dr. Vance’s recent cases. We’re examining all patients he assessed in the ER over the past two years, with a focus on misdiagnoses and inadequate care.”
She paused.
“Based on what we’re finding, I’ve placed him on administrative leave pending the completion of the review.”
“That’s a start,” I said. “But administrative leave isn’t enough. He needs to lose his license.”
“I agree,” she said quietly. “Off the record, I’ve been trying to build a case against Vance for three years.”
Her voice tightened.
“The problem is that hospital administration has been reluctant to take action because Vance brings in revenue and they’re afraid of wrongful termination lawsuits. Your son’s case might finally give us the leverage we need.”
Jeffrey filed the formal complaint with the state medical board on the fifth day of Ethan’s hospitalization.
The complaint detailed the timeline of events, the inadequate assessment, the delayed diagnosis, the preventable complications, and the pattern of similar behavior in previous cases.
He also filed a notice of intent to sue both Dr. Vance and Mercy General Hospital for medical negligence.
The hospital’s response was immediate and exactly what I’d expected.
Their legal team called Jeffrey within hours, suggesting a settlement meeting. They wanted to make this go away quietly, just like they’d done with the previous cases.
Jeffrey called me to discuss the offer.
“They’re proposing a settlement of $250,000 in exchange for a non-disclosure agreement. An agreement not to pursue the medical board complaint.”
“No,” I said.
“Garrison, that’s a substantial settlement. It would cover all of Ethan’s medical expenses and then some.”
“I don’t care about the money,” I said. “I care about making sure Vance can’t do this to anyone else. Tell them we’re proceeding with the medical board complaint and the lawsuit. No settlement, no NDA. We’re taking this public.”
There was a pause.
“You understand this means your family will be under scrutiny. Ethan’s medical records will be public. The press will likely cover this. It could be brutal.”
“I understand,” I said. “But if we take the settlement and stay quiet, Vance keeps practicing medicine and some other family ends up where we are.”
My jaw clenched.
“Except maybe their son doesn’t make it. I can’t live with that.”
The medical board investigation began six weeks later.
They assigned it to Dr. Michael Torres, an investigator with twelve years of experience reviewing physician misconduct cases.
He was thorough and professional, interviewing me, Ethan, the nurses who’d been on duty, Dr. Kowalski, and Dr. Whitmore.
He reviewed all the medical records, the timeline documentation, and the previous complaint history.
His preliminary report was damning.
It detailed multiple violations of the standard of care, including failure to perform adequate assessment, failure to order appropriate diagnostic testing, failure to document clinical reasoning, and a pattern of bias in patient care.
The report specifically noted that Vance’s treatment decisions appeared to be influenced by patient appearance rather than clinical presentation.
Vance hired his own attorney, a man named Richard Keller, who specialized in defending physicians against malpractice claims and licensing actions.
Keller’s strategy was predictable: attack the complainant’s credibility, argue that Vance’s clinical judgment was reasonable based on the information available, and claim that the outcome would have been the same regardless of when surgery was performed.
They scheduled a formal hearing for three months after the complaint was filed.
In the meantime, the story had leaked to the press.
A local investigative journalist named Christine Dalton had gotten wind of the case and started digging into Vance’s history.
What she found was worse than I’d imagined.
Over his fifteen-year career, Vance had been involved in at least twelve cases of misdiagnosis or inadequate care that resulted in patient harm. Most had been settled quietly.
A few had resulted in medical board complaints that were dismissed due to lack of evidence or closed after Vance agreed to additional training.
Christine’s article ran in the city’s major newspaper with the headline: “Pattern of neglect: how one ER doctor’s bias put patients at risk.”
It detailed Ethan’s case alongside four other cases where young patients had been dismissed by Vance as drug seekers or hypochondriacs, only to have serious medical conditions that required emergency intervention.
The public response was immediate and fierce.
Patient advocacy groups called for Vance’s license to be suspended. Other patients who’d been treated by Vance came forward with their own stories of dismissive care and missed diagnosis.
The hospital’s patient relations office was flooded with complaints.
Mercy General’s administration, facing a public relations nightmare, announced they were conducting a comprehensive review of their emergency department protocols and had terminated Dr. Vance’s employment effective immediately.
But termination from one hospital didn’t mean he couldn’t practice elsewhere.
And it didn’t address the fundamental problem of a physician whose biases made him dangerous to patients.
The medical board hearing took place on a cold morning in November, four months after Ethan’s ruptured appendix.
The hearing room was formal and intimidating, with a long table where the medical board members sat and witness chairs positioned in front.
The board consisted of five physicians and two public members, all appointed by the governor to review physician misconduct cases.
Ethan testified first.
He was nervous, his voice shaking slightly as he described his symptoms, his attempts to get treatment, and Vance’s dismissive attitude.
“He looked at me like I was trash,” Ethan said quietly, “like I wasn’t worth his time. I kept trying to explain that something was really wrong, but he’d already decided I was lying.”
Vance’s attorney cross-examined him, trying to poke holes in his timeline and suggest that Ethan had understated his symptoms or failed to communicate effectively.
But Ethan held firm, his answers clear and consistent.
The nurses testified next.
Carol Brennan was particularly effective, describing how she’d raised concerns about Ethan’s condition multiple times and been dismissed by Vance.
“In my twenty-six years as an ER nurse, I’ve learned to trust my instincts about patients,” she said. “Mr. Mills was genuinely ill. His vital signs, his appearance, his pain level—everything indicated a serious medical condition. Dr. Vance refused to listen.”
Dr. Kowalski’s testimony was clinical and devastating.
He walked the board through the surgical findings, the evidence of recent perforation, and the timeline showing that the rupture occurred during the hours Ethan was in the ER without treatment.
“In my professional opinion, if Mr. Mills had been properly assessed when he first presented to the emergency department, his appendix could have been removed laparoscopically before perforation occurred.”
He didn’t soften it.
“The delay in diagnosis and treatment directly caused the rupture and the subsequent complications, including peritonitis, and the need for open surgery, extended hospitalization, and prolonged recovery.”
Dr. Torres presented his investigative findings, including the pattern of similar incidents in Vance’s practice history.
He’d identified eighteen cases over five years where Vance had made snap judgments about patients that resulted in missed diagnoses or delayed care.
The pattern was clear.
Young patients, minority patients, patients with tattoos or unconventional appearance were disproportionately likely to be dismissed or inadequately assessed.
Then it was Vance’s turn to testify.
He sat in the witness chair looking defensive and angry, clearly resenting having to defend his clinical decisions.
His attorney had prepared him well, and his testimony hit all the expected notes.
He’d used his best clinical judgment based on years of experience. Emergency medicine required quick decision-making with limited information. Not every patient with abdominal pain required extensive testing. He’d followed the standard of care.
But under cross-examination by the medical board’s attorney, his testimony fell apart.
“Dr. Vance, your physical exam notes for Mr. Mills state mild tenderness on palpation, but three nurses documented that the patient was in severe distress and had difficulty lying flat due to pain. How do you explain the discrepancy?”
Vance shifted in his chair.
“Patients often exaggerate their symptoms. Part of clinical judgment is distinguishing between subjective complaints and objective findings.”
“So you believed three experienced nurses were wrong about their assessment of the patient’s distress level?”
“I believed my own physical examination findings.”
“Your physical examination that lasted approximately ninety seconds according to nursing documentation.”
Vance’s jaw tightened.
“I performed an adequate examination.”
“Did you assess for rebound tenderness?”
“I don’t recall specifically.”
“Did you assess for rigidity or guarding?”
“As I said, I don’t recall the specific details of the examination.”
The attorney’s voice stayed steady.
“Dr. Vance, you documented that Mr. Mills appeared to be exhibiting drug-seeking behavior. What specific behaviors led you to that conclusion?”
He hesitated.
“The patient was requesting pain medication. He seemed overly focused on getting narcotics.”
“According to the nursing notes, Mr. Mills never specifically requested narcotics. He asked for pain relief after being in the ER for three hours with worsening symptoms.”
The room felt smaller.
“Is asking for pain management after three hours of acute abdominal pain indicative of drug-seeking behavior?”
“In my experience, genuine medical emergencies present differently.”
“How so?”
Vance swallowed.
“The patient’s demeanor, his appearance, his communication style—all suggested someone who was drug-seeking rather than genuinely ill.”
“Could you be more specific about his appearance?”
Vance realized too late that he’d walked into a trap.
“He had tattoos, piercings—unconventional appearance.”
“And in your medical training,” the attorney asked, “were you taught that tattoos and piercings are contraindications for serious medical conditions?”
The hearing room was dead silent.
Vance’s face flushed.
“Of course not. But emergency physicians develop instincts about patients.”
“Instincts based on appearance rather than clinical presentation.”
“That’s not what I said.”
“But that is what you did, isn’t it, Dr. Vance? You looked at a young man with tattoos, made an assumption about his character, and provided inadequate care based on that assumption rather than on his actual symptoms.”
The medical board deliberated for two hours.
When they returned, the chairman, Dr. William Foster, read their decision.
“After careful review of the evidence, testimony, and investigative findings, this board finds that Dr. Leonard Vance violated multiple standards of medical practice in his treatment of Mr. Ethan Mills.”
He didn’t rush.
“Specifically, Dr. Vance failed to perform an adequate physical examination, failed to order appropriate diagnostic testing despite clear clinical indicators, allowed personal bias to influence medical decision-making, and demonstrated a pattern of similar conduct in other cases.”
He looked directly at Vance.
“These violations constitute serious professional misconduct that endangered patient safety. Dr. Vance, it is the decision of this board to revoke your medical license effective immediately.”
He continued, voice firm.
“You are prohibited from practicing medicine in this state. Additionally, we are forwarding our findings to the National Practitioner Data Bank to ensure this information is available to other state medical boards should you attempt to obtain a license elsewhere.”
Vance’s face went white.
His attorney immediately stood up, objecting, requesting reconsideration, but the board chairman cut him off.
“The decision is final. This hearing is adjourned.”
I watched Vance gather his papers with shaking hands and walk out of the hearing room.
His career was over.
His reputation was destroyed.
And most importantly, he would never have the opportunity to harm another patient the way he’d harmed my son.
Outside the hearing room, Christine Dalton was waiting with a camera crew.
“Dr. Mills, how do you feel about the board’s decision?”
I looked directly at the camera.
“I feel that justice was served, but I also feel angry that it took my son nearly dying to force the system to act.”
I didn’t soften what came next.
“Dr. Vance had a pattern of negligent care going back years. The hospital knew about it. The medical board had received complaints, but nothing was done until someone with enough resources and knowledge to fight back got involved.”
My voice stayed level.
“How many other patients were harmed because the system protected a bad doctor instead of protecting patients?”
The story aired that evening on every local news channel and was picked up by national health policy outlets.
It sparked a broader conversation about bias in medical care, about how hospitals handle problem physicians, and about the need for stronger accountability mechanisms.
Three months after the medical board hearing, Mercy General Hospital settled our lawsuit for $1.8 million.
But more importantly, they implemented new protocols for ER assessments, mandatory bias training for all staff, and a patient advocate position specifically focused on addressing complaints about inadequate care.
Six other patients who’d been harmed by Vance filed their own lawsuits and medical board complaints.
The hospital settled all of them and terminated two administrators who’d been involved in covering up previous complaints.
Ethan made a full recovery, though he had a surgical scar and some lingering anxiety about medical care.
He finished his master’s degree and now works for the EPA doing environmental impact assessments for development projects.
He still has the tattoos and piercings, and he still gets judgmental looks from some medical providers.
But he’s learned to advocate for himself, to demand appropriate care, and to walk out if a doctor isn’t listening.
One year after the incident, I was invited to speak at a national conference on medical ethics.
I told Ethan’s story to an auditorium full of physicians, medical students, and healthcare administrators.
I showed them the timeline, the missed opportunities, the consequences of bias.
“Every patient deserves to be assessed based on their symptoms, not their appearance,” I said. “Every patient deserves a physician who will put aside assumptions and do the clinical work required to reach an accurate diagnosis.”
I let the silence do some of the work.
“And every physician who fails to meet that standard should face consequences, not protection from an institution more concerned with liability than patient safety.”
The speech was recorded and used in medical schools across the country as a case study in implicit bias and standard of care violations.
I received hundreds of emails from patients who’d had similar experiences, who’d been dismissed or inadequately treated because they didn’t fit the image of what a “real patient” should look like.
Ethan and I started a patient advocacy organization focused on helping people navigate medical complaints and hold negligent providers accountable.
We worked with attorneys, medical board investigators, and patient rights groups to create resources for people who’d been harmed by medical negligence but didn’t know how to fight back.
Dr. Vance tried to get his license reinstated twice.
Both times, the medical board denied his petition.
Last I heard, he was working as a consultant for a medical malpractice insurance company, reviewing cases to help them deny claims.
The irony wasn’t lost on anyone.
Two years after that phone call at 3:47 a.m., I sat in my office at St. Catherine’s Hospital reviewing the surgical schedule, and my phone rang.
For a moment, my chest tightened with the old fear.
But it was just Ethan calling to tell me about a grant he’d received for his research.
We talked for twenty minutes about his work, his life, his plans for the future.
Before we hung up, he said something that made my throat tighten.
“Dad, I never thanked you properly—for believing me, for fighting for me, for making sure what happened to me didn’t happen to anyone else.”
“You don’t need to thank me,” I said. “That’s what fathers do.”
But as I ended the call and looked out my office window at the city below, I thought about all the patients who didn’t have someone to fight for them.
All the people who were dismissed, ignored, or inadequately treated because they didn’t have power or resources or knowledge.
The system had failed Ethan, but he’d survived because I had the expertise and position to force accountability.
That wasn’t justice.
That was privilege.
Real justice would be a system that protected all patients equally, regardless of who their father was.
We weren’t there yet.
But every complaint filed, every bad doctor held accountable, every protocol changed moved us closer.
Ethan’s near-death experience had exposed one corrupt physician and forced one hospital to improve its standards.
That was something.
It wasn’t enough, but it was something, and I was going to keep fighting until the something became everything.